On the evening of Friday, Oct. 31, the Centers for Medicare & Medicaid Services (CMS) posted the 2026 Medicare Physician Fee Schedule (MPFS) final rule. Following is ASNC’s preliminary analysis.
Be on the lookout for additional reporting on specifics that may impact your practice; actions ASNC will take; and ASNC’s payment charts, which will compile the reimbursement rates for all nuclear cardiology services. We will also notify you when CMS posts the 2026 Hospital Outpatient Prospective Payment System (HOPPS) final rule, which could be any day.
Efficiency Adjustment
The rule finalizes a negative 2.5 percent efficiency adjustment that will be applied to the vast majority of physician services, including diagnostic imaging procedures. CMS was not swayed by comments from ASNC and others opposing the blanket adjustment. The agency maintains that current valuations for the most services do not account for efficiencies gained over time.
- The -2.5 percent efficiency adjustment will be applied to the work RVUs and corresponding intraservice portion of physician time for non-time-based services. The only change CMS made from the policy in the proposed rule was exempting codes new for 2026.
- CMS used the Medicare Economic Index productivity adjustment percentage with a look-back period of 5 years to calculate the efficiency adjustment.
- CMS intends to apply the efficiency adjustment every 3 years with no floor on how much a service could be devalued.
Conversion Factors
For 2026, there are 2 conversion factors. Which conversion factor applies to you depends on whether you are an alternative payment model qualified participant (APM QP).
- Non-APM QP Conversion Factor: $33.4009 (+3.26 percent change from 2025)
- APM QP Conversion Factor: $33.5675 (+3.77 percent change from 2025)
The conversion factors reflect statutory adjustments, including the 2.5 percent positive adjustment provided by Congress earlier this year, a positive 0.49 percent budget-neutrality adjustment resulting from misvalued code changes, and the negative 2.5 percent efficiency adjustment.
Practice Expense
The final rule rejects the American Medical Association’s Physician Practice Information Survey for updating 2026 practice expense (PE) relative values and instead reduces the physician’s indirect PE payment for services provided in a facility, even if the physician is not employed by the hospital.
CMS says its new PE policy reflects the increased number of physicians practicing in hospital-owned practices and employed directly by hospitals while supporting site-neutrality goals.
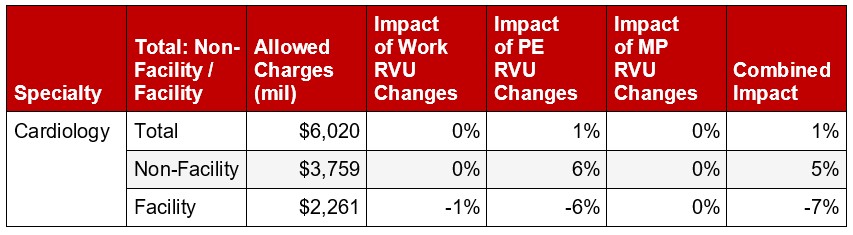
The new PE methodology will not apply to nuclear SPECT or PET services; however, it will affect cardiology MPFS payments overall. Office payments will increase by 5 percent, and MPFS payments for services provided in facilities will decrease by 7 percent.
Cardiology Overall Impact Chart:
Lawmakers Need to Hear from You: Sign up for ASNC’s Capitol Hill Days
Medicare physician payment reform will remain a top advocacy priority for ASNC in 2026. Lawmakers need to hear directly from you about why physicians deserve a Medicare payment system that is fair, appropriately reflects the cost of providing care, and is free of unnecessary regulatory burden. Join ASNC leaders on Capitol Hill for meetings with congressional lawmakers, May 4-5, 2026. Space is limited.
Article Type
News & Announcements
Category
Advocacy
Related Posts
CMS Names Physicians Required to Participate in New Heart Failure Payment Model
The Centers for Medicare & Medicaid Services (CMS) has released a searchable…
Immediate Impact! ASNC Statement Driving Cardiac PET Adoption Across the United States
“ASNC’s Clinical Indications for PET statement got the attention of our hospital…
This Legislation Would Halt Pay Cut Now Impacting Most Physician Services
“The 2.5% reduction to work RVUs – the so-called ‘efficiency adjustment’ –…