Tell CMS This Proposal Must Not Be Finalized
The Centers for Medicare & Medicaid Services (CMS) is proposing a change that would result in a 57 percent cut to payments for the code used in amyloid imaging. The agency wants to reassign the amyloid imaging CPT code 78803 to a new ambulatory payment classification (APC) starting in 2026.
ASNC is calling on all members to write to CMS with the message that this proposal must not be finalized.
The deadline to submit comments to CMS is Monday, Sept. 15.
Take Action Now! CMS Must Hear from You by Monday, September 15
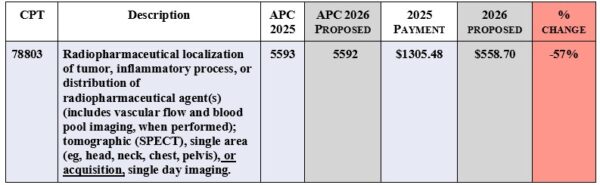
Chart showing CMS proposed cut to amyloid imaging code
The fastest and easiest way to send comments to CMS is through the ASNC Action Center. ASNC has provided template letter for you to personalize with information about the devastating impact that this cut of 57 percent would have on your practice and your patients.
Article Type
News & Announcements
Category
Advocacy
Related Posts
Immediate Impact! ASNC Statement Driving Cardiac PET Adoption Across the United States
“ASNC’s Clinical Indications for PET statement got the attention of our hospital…
This Legislation Would Halt Pay Cut Now Impacting Most Physician Services
“The 2.5% reduction to work RVUs – the so-called ‘efficiency adjustment’ –…
Manufacturer Shares Update on HMDP Supply
ASNC is staying in touch with radiopharmaceuticals manufacturers that were expecting shortages…



