In the 2026 Medicare Physician Fee Schedule proposed rule released July 14, the Centers for Medicare & Medicaid Services (CMS) proposed a 0.55 percent increase to the conversion factor, which would be in addition to positive statutory adjustments.
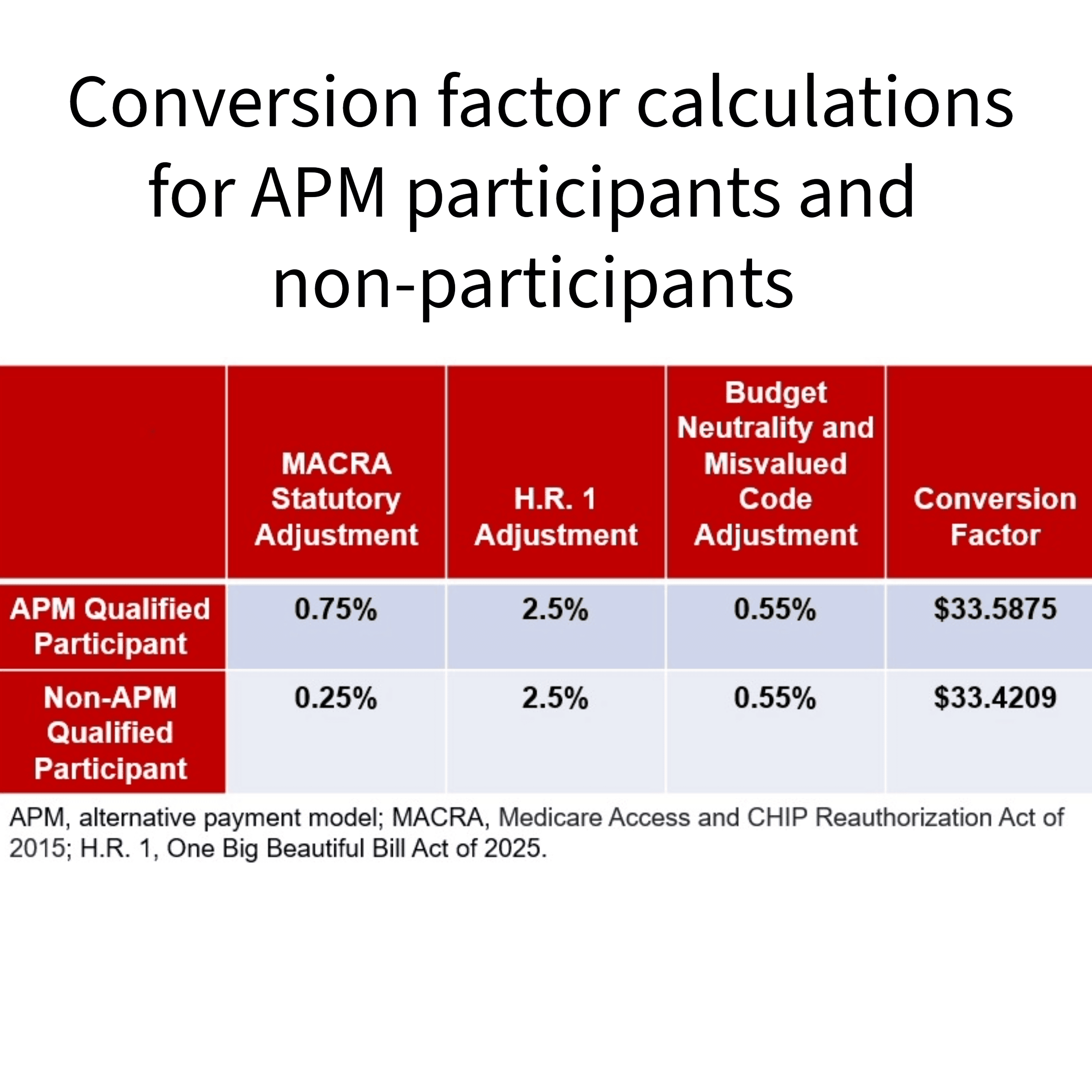
CMS is also proposing to use different conversion factors for clinicians who participate in an alternative payment model (APM) versus those who do not. APM participants would receive a 0.75 percent update to the conversion factor applied to services they provide while those not participating in an APM would receive a 0.25 percent update. This is in addition to the 1-year positive payment update of 2.5 percent included in H.R 1, the One Big Beautiful Bill Act of 2025.
It is important to note that the increases to the conversion factor would be muted by two new proposed policies that would negatively affect nuclear cardiology:
- A proposed efficiency adjustment for non-time-based services, and
- A revised practice expense methodology for facility-based services.
Keep reading – ASNC’s analysis of both proposals is below.
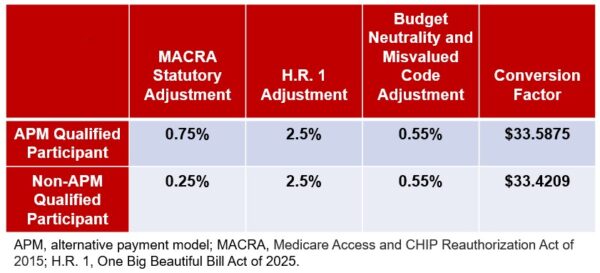
Overview of how the conversion factor would be calculated for APM participants and non-participants.
CMS’s Efficiency Adjustment Proposal
CMS proposes to apply a new “efficiency adjustment” of -2.5 percent to work relative value units (RVUs) and the corresponding intraservice portion of physician time of non-time-based services. The proposal is based on CMS’s assumption that both the intraservice portion of physician time and the work intensity would decrease as a practitioner develops expertise in performing the specific service. CMS’s stance is that the current RVUs may not reflect these efficiencies due to the infrequency of service revaluation under the physician fee schedule and the limitations of reliance on survey data.
The efficiency adjustment would apply to all codes except time-based codes, including E/M visits, care management services, behavioral health services, and services on the CMS telehealth list. The new efficiency adjustment would impact most surgical specialties, radiology, and pathology by reducing overall payment by 1 percent.
To calculate the efficiency adjustment, CMS proposes using the Medicare Economic Index (MEI) productivity adjustment with a look-back period of 5 years. For 2026, CMS would sum all productivity adjustments included in the MEI updates from 2022 to 2026. If finalized, CMS proposes to apply the efficiency adjustment to the intraservice portion of physician time and work RVUs every 3 years.
CMS’s Proposed Approach for Calculating Practice Expense
CMS is proposing to modify the indirect practice expense methodology to redistribute indirect practice costs from facility-based services to non-facility-based services. For each service valued in the facility setting, for 2026, CMS proposes to reduce the portion of the facility practice expense RVUs allocated based on work RVUs to half the amount allocated to non-facility practice expense RVUs.
This change in practice expense methodology would result in a dramatic shift of payment between sites of service. CMS chose this methodology over using American Medical Association Physician Practice Information Survey information to update practice relative values. CMS says the original practice expense allocation methodologies that assumed physicians maintained separate practice locations even if they furnished some care in hospitals do not reflect the decline in the number of physicians working in private practice.
ASNC has significant concerns with CMS’s proposal and is focused on ensuring that reimbursement for services provided in the facility setting adequately reflects practice costs.
Ask Your Questions at ASNC2025
Considering the complexity of CMS’s proposed changes to reimbursement policies, it is more important than ever for you and your team to stay current on health policy issues. Be sure to attend ASNC2025‘s Radioactive Revenue session, where experts from ASNC’s advocacy team will explain how the updates in the proposed rules will affect nuclear cardiology services.

Faculty for ASNC2025’s Radioactive Revenue session.
This ASNC2025 session will also cover documentation guidelines to help you avoid prior authorization hassles and unnecessary claim denials. Plus, practical guidance on how to be an effective advocate at local and national levels! This session is recommended for all U.S.-based cardiac imagers and their billing teams.
ASNC2025 will be held Sept. 4-7 in Orlando, Florida. Choose in-person or virtual registration.
Article Type
News & Announcements
Category
Advocacy
Related Posts
This Legislation Would Halt Pay Cut Now Impacting Most Physician Services
“The 2.5% reduction to work RVUs – the so-called ‘efficiency adjustment’ –…
Manufacturer Shares Update on HMDP Supply
ASNC is staying in touch with radiopharmaceuticals manufacturers that were expecting shortages…
Medicare Telehealth Flexibilities Expire as Federal Government Partially Shuts Down
Congress’s failure to pass the remaining 6 fiscal year 2026 spending bills,…