ASNC is nuclear cardiology's voice on health policy matters and the principal advocate for professionals in the field. ASNC's advocacy team tackles issues impacting nuclear cardiology at every level, including legislative and regulatory concerns, state-level policies, third-party coverage challenges, and beyond. With your support and participation, ASNC has been instrumental in passing key federal legislation, delaying the AUC mandate, and preserving fair reimbursement for nuclear cardiology services.
Your engagement is critical to our continuing success. You can help ASNC advocate on behalf of your practice and your patients by staying current on health policy issues, responding to calls to action, and keeping your membership current.
New
Now Available On-Demand: Nuclear Cardiology Reimbursement 2026 Webinar Recording
You must be logged in to view this content.
ASNC relies on a team of physician experts who ensure nuclear cardiology is well represented in key policymaking arenas throughout the House of Medicine.

American Medical Association Relative Value Update Committee, aka 'The RUC'
In addition to chairing ASNC's Health Policy Committee, Friederike Keating, MD, FASNC, represents ASNC as an advisor on the American Medical Association's Relative Value Update Committee.
Also known as "the RUC," this body makes recommendations to the Centers for Medicare & Medicaid Services (CMS) on the relative values assigned to new or existing CPT codes. While CMS is not required to follow the RUC's recommendations, the committee plays a crucial role in helping the federal government determine the value of medical services in patient care.
American Medical Association CPT Advisory Committee
Edward Hulten, MD, MPH, FASNC, will represent ASNC on the American Medical Association's CPT Advisory Committee, which supports the AMA's CPT Editorial Panel. The panel meets regularly to revise, update, or modify CPT codes, descriptors, rules, and guidelines used in medical billing and reporting. The committee may advise the panel on procedure coding, nomenclature, and appropriateness; suggest changes to the code set; and support education on coding issues.
Dr. Hulten’s appointment will be finalized at the panel's April 2025 meeting.


American Medical Association House of Delegates
Suman Tandon, MD, FASNC, and Ahmet Oktay, MD, are ASNC's representative to the American Medical Association’s House of Delegates (HOD). The AMA HOD is the AMA's legislative and policymaking body, which meets twice per year to determine AMA policy. At HOD meetings, Drs. Tandon and Oktay speak on issues of importance to nuclear cardiology practice and vote on issues in accordance with ASNC’s policy priorities.
American College of Cardiology Imaging Section Leadership Council
ASNC Past President Dennis A. Calnon, MD, MASNC, is ASNC’s representative to the American College of Cardiology Imaging Section Leadership Council. This group of representatives from the major cardiovascular imaging modalities meets regularly to discuss policy issues affecting cardiology as a whole and imaging specifically and to offer input on the coordination of imaging activities in the College.
American Medical Association Collaborative on Artificial Intelligence
As the chair of ASNC's Artificial Intelligence Task Force, Jamieson M. Bourque, MD, MHS, FASNC, represents nuclear cardiology on the American Medical Association's Collaborative on Artificial Intelligence.
The AMA's AI Collaborative facilitates regular contact across societies for sharing of information on how AI technologies are affecting the practice of medicine today and in the future.
This Legislation Would Halt Pay Cut Now Impacting Most Physician Services
“The 2.5% reduction to work RVUs – the so-called ‘efficiency adjustment’ –…
Manufacturer Shares Update on HMDP Supply
ASNC is staying in touch with radiopharmaceuticals manufacturers that were expecting shortages…
Medicare Telehealth Flexibilities Expire as Federal Government Partially Shuts Down
Congress’s failure to pass the remaining 6 fiscal year 2026 spending bills,…
Policy Priorities
ASNC and its members play crucial roles in policy decisions affecting the practice of nuclear cardiology. ASNC's policy priorities include ensuring fair and appropriate reimbursement and health coverage, ensuring patients' access to appropriate imaging services, reducing prior authorization and administrative burden on practices, monitoring for medical isotope supply challenges, and participating in efforts to reform physician payment systems.

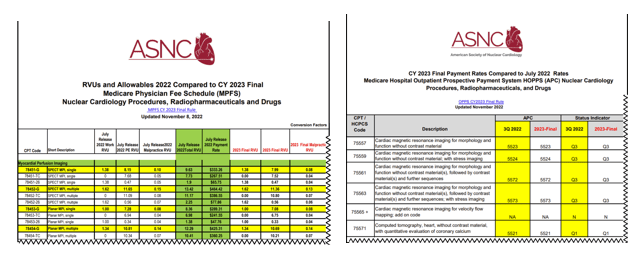
Navigating coverage and reimbursement can be a challenging task for all physicians. Nuclear cardiology faces unique payment and practice management issues in both the public and private sectors. Find ready-made payment charts made specifically for ASNC members and summaries of important developments in nuclear cardiology reimbursement.
Advocacy: Take Action
ASNC highlights time-sensitive news about health policy and advocacy issues that affect the delivery of quality cardiovascular care. As an ASNC member, you will receive advocacy alerts about reimbursement and coverage policies, coding instructions, medical isotope supply, and about other time-sensitive issues. These alerts will keep you current on important matters impacting your profession, your practice, and your patients. They will also detail how you can help.
ASNC’s grassroots advocacy works! With member support, ASNC has been instrumental in passing key legislation, delaying the AUC mandate, reducing the prior authorization requirements of some payers, improving coverage policies, and preserving fair reimbursement for nuclear cardiology services.
ASNC’s Advocacy Action Center makes it easy for you to lend your support for vital campaigns.