ASNC is your source for the latest information emerging from the field of nuclear cardiology and cardiac imaging.
From our flagship scientific journal to our weekly newsletter, ASNC is dedicated to delivering high-quality research, news, and updates from the field.
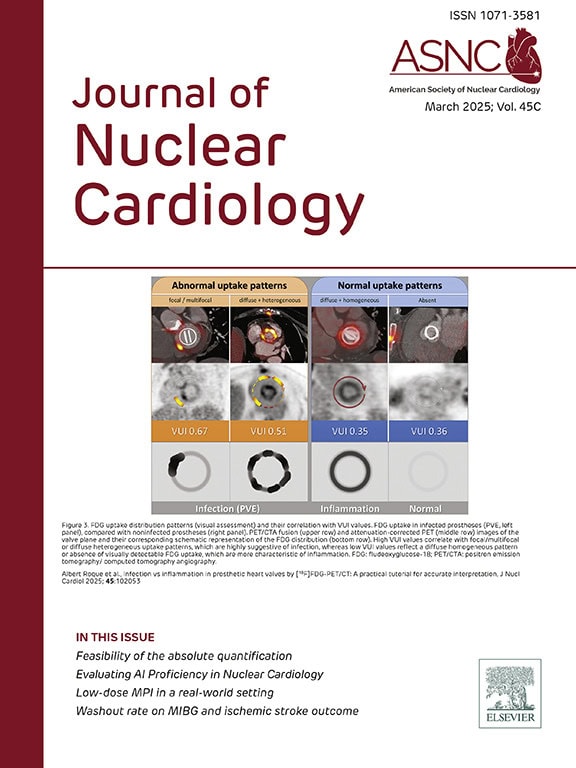
Journal of Nuclear Cardiology
The Journal of Nuclear Cardiology (JNC) is the only journal in the world devoted to this dynamic and growing subspecialty. The JNC is the official peer-reviewed publication of ASNC featuring the latest research findings and clinical developments in nuclear cardiology and related fields.
Read the latest issue of the Journal of Nuclear Cardiology (JNC). Full access to the JNC is available with an ASNC Membership. Join or renew today!
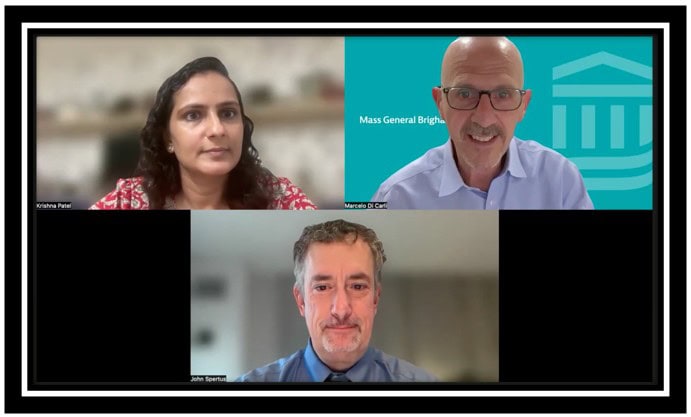
The JNC CardioConnect podcast links experts, insights, and innovations in nuclear cardiology. Join Editor-in-Chief Marcelo F. Di Carli, MD, MASNC, and authors as they discuss important articles from the Journal of Nuclear Cardiology (JNC).
Access the latest news and updates from ASNC. Search by category of interest, date, and more.
Podcast: Nuclear Cardiology Needs to Close This Workflow Gap Now
Even as nuclear cardiology is advancing at breakneck speed with new technology,…
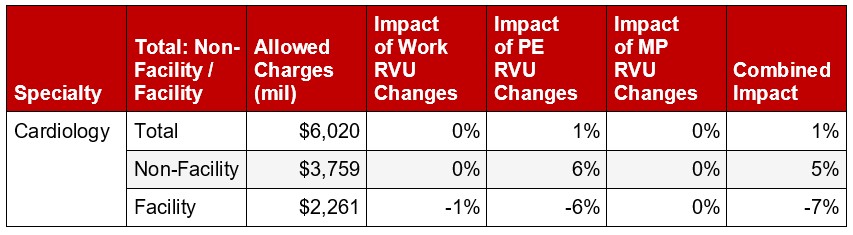
CMS Releases 2026 Medicare Physician Fee Schedule Final Rule
On the evening of Friday, Oct. 31, the Centers for Medicare &…
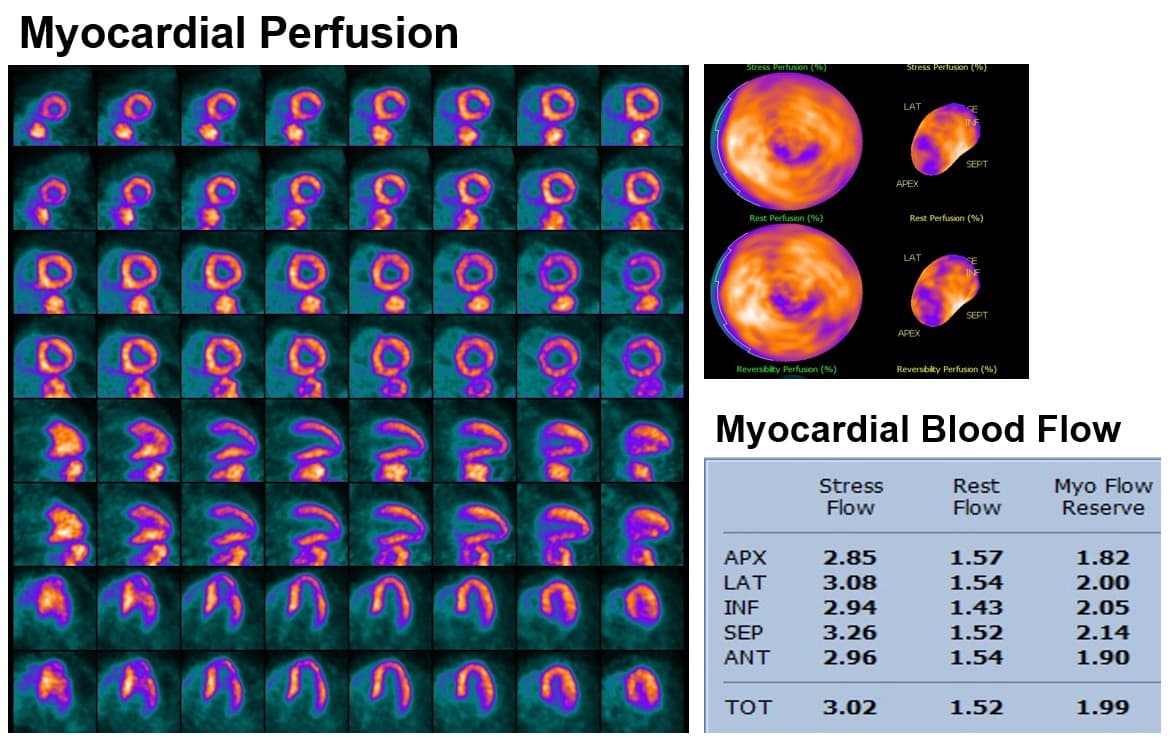
Woman, Age 52, Presents with NSTEMI. What Is Her Diagnosis?
The patient featured in this month’s cardiac PET case challenge is a…
Sign up to receive ASNC's bi-weekly round-up of news and information related to nuclear cardiology and cardiovascular imaging.
ASNC Interview Series
Explore the latest topics in nuclear cardiology through video conversations with luminaries and key leaders in the field.
Advertising
ASNC is where your marketing investment reaches the right audience and achieves optimal return.